Patient Information from ISHA – The Hip Preservation Society
Perthes Disease – Later Management in Adults
Perthes Disease – Later Management in Adults
Definition
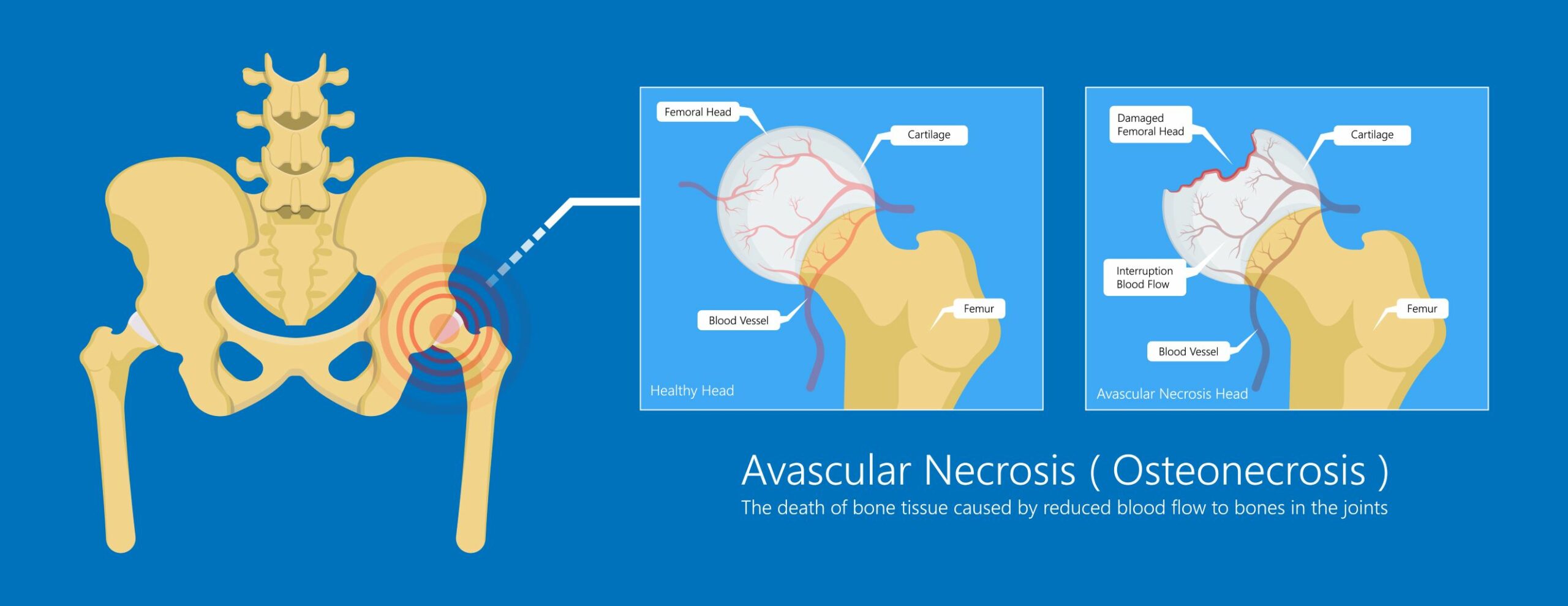
Perthes is a childhood form of avascular necrosis (AVN), where temporary interruption of blood supply to the femoral head may result in varying degrees of damage to the joint. Unlike in adults, the interruption to the blood supply in children with Perthes does eventually recover spontaneously, with the process taking between two and five years. A misshapen femoral head and acetabulum which results from this bone damage may affect joint function and stability, with the onset of osteoarthritis and other conditions of varying severity requiring treatment in later years.
Signs and Symptoms
Adults who experienced Perthes as children may present with a range of deformities around the hip joint, including femoroacetabular impingement (FAI), or labral, cartilage and ligament tears. These may contribute to instability and associated loss of movement and function. If diagnosed before the onset of any joint degenerative changes, joint preservation treatment is more likely to be effective, and will hence delay the onset or progression of osteoarthritis and the consequent need for a hip replacement. Some treatments are discussed below.
Diagnosis
Before agreeing a treatment plan, consultation with a hip preservation surgeon will involve a thorough clinical examination. It is likely that imaging including a combination of X-rays, MRI, CT or ultrasound scanning will be required before establishing the causes of presenting symptoms and difficulties.
Non-Surgical Treatment
Physiotherapy may be helpful, including activity modification, pain management, overall postural awareness and improvement, and exercises aimed at improving any muscle imbalances and weakness.
Weight management, nutritionist input, cessation of smoking and general lifestyle advice may also be helpful in managing symptoms conservatively.
Interventional radiology using image guided local anaesthetic, corticosteroid or other biologics injections in and around the hip joint may be suggested in conjunction with other conservative measures.
Surgical Treatment
Hip preservation surgery may be arthroscopic (assuming the area requiring attention is accessible using this approach) or open. The overall aim of any procedure will be to improve coverage of the femoral head by the acetabulum, restoring stability and aiming to reduce pain and improve function. Treatment of any other conditions, including repair of labral tears and attention to any cartilage damage, can take place at the same time.
The orientation of the acetabulum may require altering and/or the surface area of the acetabulum may need increasing to improve coverage of the femoral head. This may be achieved via a range of procedures, including proximal femoral osteotomy, periacetabular osteotomy, femoral osteochondroplasty, or trochanteric flip osteotomy. In young adults, a triple pelvic osteotomy (periacetabular osteotomy – also called PAO) to reorientate the femoral head, if required, would be performed by a young adult hip preservation specialist.
A total hip replacement may be offered where degenerative changes in the articular cartilage resulting from deformities in the joint from Perthes are too extensive for joint preservation to be effective.
What to expect after surgery

This will vary depending on the age of the patient, what surgery was performed, and the preferences and recommendations of the treating hip preservation surgeon. Following many of these procedures, there is likely to be a lengthy period of rehabilitation.
There may be limitations to weightbearing and activities during the first two or three months. These will vary amongst surgeons and will depend on operative findings and techniques performed.
Physiotherapy can begin immediately after surgery, gradually increasing range of movement, stability, strength, mobility, and function over a period of six to twelve months, depending on the surgery performed and individual aims.