Patient Information from ISHA – The Hip Preservation Society
Lateral Hip Pain, including Greater Trochanteric Pain Syndrome
Lateral Hip Pain, including Greater Trochanteric Pain Syndrome
Definition
Lateral hip pain (pain down the side of the upper thigh) can result from a range of conditions and injuries, including some elements of snapping hip syndrome, such as proximal iliotibial band syndrome, trochanteric bursitis, and gluteal tendinopathy. These conditions, which may also be known as “greater trochanteric pain syndrome (GTPS)”, tend to be more common in females aged between 40 and 60 years of age.
Proximal Iliotibial Band Syndrome
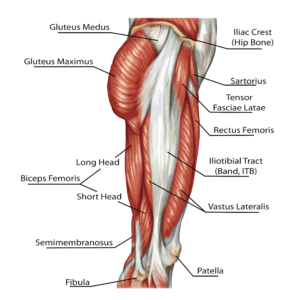
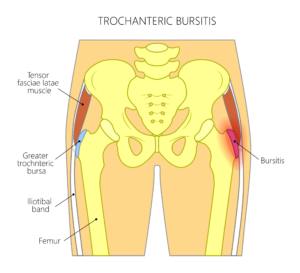
Anatomically, the iliotibial tract (iliotibial band tract or iliotibial band – ITB) extends from the outer edge of the pelvis down to the outer side of the knee. Structurally, the ITB is a thickened band of tissue, which can be damaged or injured as a result of overuse, trauma or inflammation, and associated degenerative changes, including GTPS. This is turn may be related to greater trochanteric bursitis (see adjacent) and/or hip abductor tendon damage (see below).
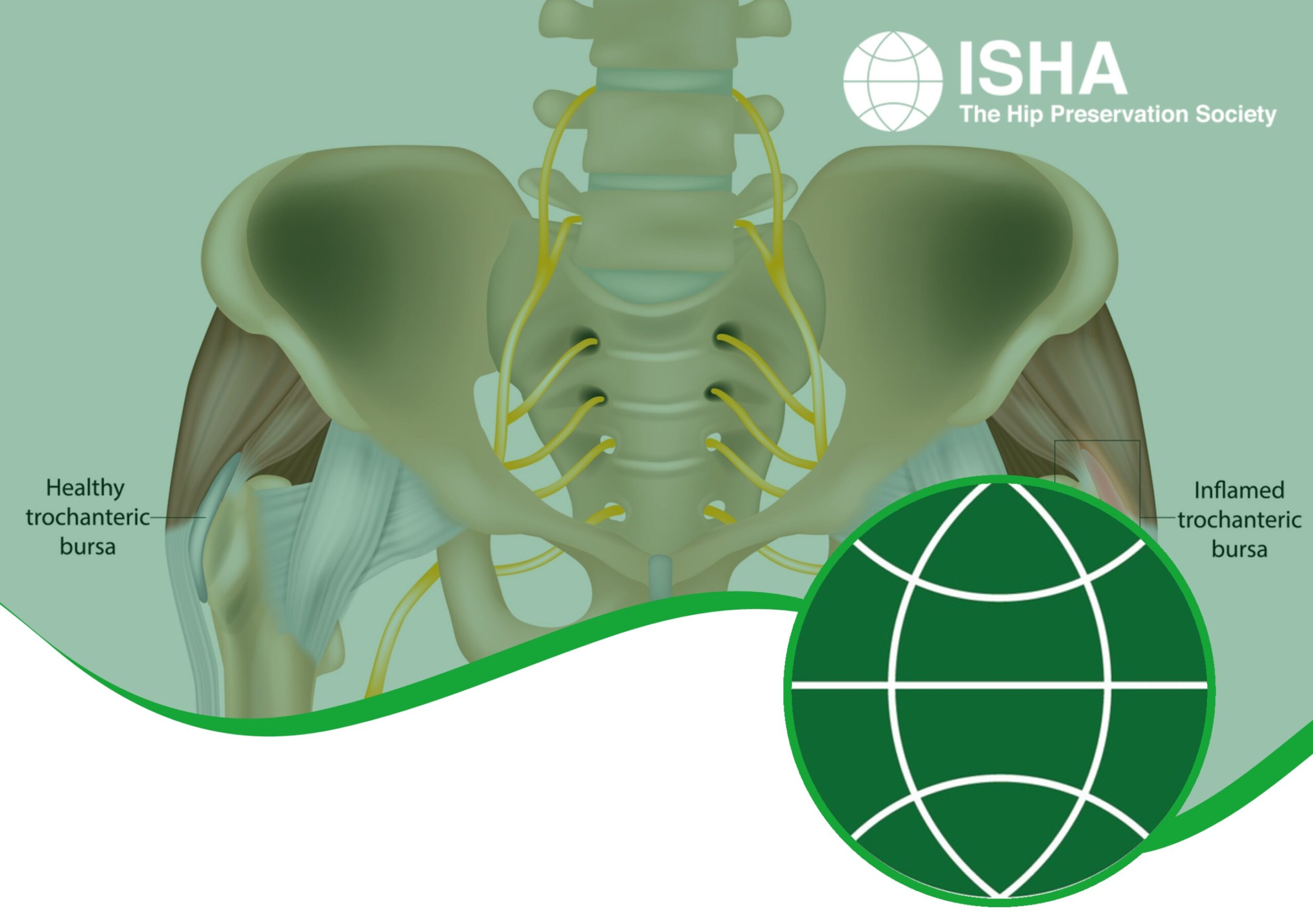
Trochanteric Bursitis
This condition results from inflammation affecting one or more of the bursaes, of which there are nine, located at the side of the hip, all very close to the greater trochanter. Around the body, bursaes, which are small sacs of fluid, reduce friction caused by the movement of soft tissues over bony points. They have a concentrated nerve supply, hence can become very painful once inflamed. As there are multiple structures passing and attaching around the side of the hip, the cause of pain in that area can be difficult to isolate, and often bursitis here is closely related to pain resulting from gluteal tendinopathy. The large number of bursae further complicates any diagnosis.
Gluteal Tendinopathy
Tendinopathy describes a range of tendon conditions, including tendinosis – where degenerative changes to the collagen (tendon tissue) have occurred, caused by repetitive overloading of the tendons. This breakdown or deterioration in tendon tissue can result in tears to the gluteal tendons, most often affecting the gluteus medius and gluteus minimus tendons close to or where they attach to the greater trochanter. Damage can range from minor, very small tears to complete rupture of the tendon, and will not generally heal with rest and non-surgical treatment, although some relief of symptoms may be possible. Tendinopathy should be differentiated from tendinitis, which is not thought to result in degenerative breakdown of tissue but is characterised by small micro-tears from repetitive movements, which may repair over time.
Signs and Symptoms
- Pain down the side of the hip along the outside of the thigh, extending in some cases to the knee
- Pain aggravated by activities including laying on the affected side, walking or stair climbing
- Swelling around the outside of the hip
- Tenderness to touch
- Pain when sitting cross legged
- Limping
Diagnosis
A detailed history of symptoms together with a physical examination may provide information suggesting the cause of any lateral hip pain. Imaging including MRI, X-rays and diagnostic injections may provide additional information. It is worth noting that imaging does not always reveal enough information to enable a definitive diagnosis. Where all non-surgical treatment options have been exhausted, a hip arthroscopy may be suggested to explore the hip and surrounding structures. Treatment of affected structures could be performed during the same arthroscopy, after a complete exploration of the area.

Non-Surgical Treatment
- Physiotherapy, which may include tailored exercise regimes, activity modifications, gait training, soft tissue massage, shockwave treatment, and postural advice, all aiming to reduce load and compression around the side of the hip
- Corticosteroid injections
- Platelet rich plasma (PRP) injections, which may help promote soft tissue healing
Surgical Treatment
Where non-surgical options fail to alleviate symptoms, surgical management may be suggested, via either an open or arthroscopic approach. A range of procedures can be performed dependent on the structures affected, and may include one or more of the following:
- Bursectomy – removal of an inflamed bursa(e)
- Repair to any significant gluteal tendon tears
- Removal of adhesions caused by chronic inflammation
- Release of any tight tissues, including the iliotibial band (ITB)
What to expect after surgery
Recovery following arthroscopic surgery is generally quicker than after an open procedure and hence returning to activities is also easier. Any return to sport will also depend on operative findings, and advice will be provided by the treating hip preservation surgeon and physiotherapist.
There may be limitations to weightbearing and activities during the first two or three months, which will vary amongst surgeons and will depend on operative findings and techniques performed.
Physiotherapy can begin immediately after surgery, gradually increasing range of movement, stability, strength, mobility and function over a period of up to six months, depending on the surgery performed and individual aims.