Patient Information from ISHA – The Hip Preservation Society
Chondral Lesions and Osteochondral Defects
Chondral Lesions and Osteochondral Defects
Definition
The hip joint has articular surfaces covering the head of the femur and the socket (acetabulum). These surfaces are covered with hyaline cartilage, which enables the joint to move freely with reduced friction. Damage may occur to either the femoral head or the acetabulum affecting either: only the articular cartilage, resulting in a chondral lesion, or both the cartilage and the underlying bone, resulting in an osteochondral defect.
Both chondral and osteochondral defects more commonly affect the acetabulum and tend to develop following a traumatic event, such as a direct blow to the hip in a fall or car accident. These conditions may also develop over time due to repetitive movements, overuse and stress from sports and other activities. Often this latter form of cartilage damage occurs in relation to other hip disorders, including hip dysplasia and femoroacetabular impingement.
Cartilage does not have the ability to heal itself, so chondral lesions which cause symptoms may require surgery. Osteochondral defects, however, may have some healing properties due to the possible release of stem cells from bleeding that occurs following damage to the bone. Where symptoms do not settle, surgery may also be needed.
Surgery is aimed at repairing the damaged area by encouraging the growth of scar tissue (or fibrocartilage), which, whilst not as good quality as the original hyaline cartilage, may act as a good substitute, offering ongoing protection and reducing pain. This may serve to prevent or delay the onset of osteoarthritis.
Signs and Symptoms
These will vary depending on the depth of the cartilage damage. The deeper the defect, the more noticeable the symptoms will be. Symptoms may include the following:
- Pain
- Joint swelling
- Synovitis
Mechanical symptoms such as locking or instability may result from loose fragments of cartilage affecting movement of the joint.
Diagnosis
A thorough history will be taken from the patient alongside a physical examination. Imaging is likely to begin with X-rays to view the joint and bone structure. This may be followed up with MRI, magnetic resonance arthrogram (MRA) or CT scanning. Chondral and osteochondral defects can be difficult to see on imaging and a hip arthroscopy may be needed to confirm the source of any symptoms. Any defect or damage can then be treated. Treatment for chondral and osteochondral defects tends to only be advised where there are no signs of more general degenerative changes or evidence of osteoarthritis.
Non-Surgical Treatment
In the first instance, the following may help relieve symptoms and enable a return to activity:
- Rest and limitations of sporting activities
- Hyaluronic acid injections
- PRP injections
Surgical Treatment
Chondral Lesions
There are a range of surgical treatments (Dallich et al, 2019), which will vary between surgeons and countries. Some are described below:
- Chondroplasty – removal of any loose fragments, and smoothing of loose flaps of cartilage to avoid them becoming displaced.
- Microfracture – before microfracture is performed, a chondroplasty is usually completed to ensure that any unstable areas of cartilage have been tidied. Microfracture is a marrow stimulating procedure, encouraging stem cells from the bone marrow up to the surface where any damage exists, promoting the growth of scar tissue (fibrocartilage). Fibrocartilage does not have the same properties as hyaline cartilage and eventually it will fail, leading to further damage and the onset of osteoarthritis. More recent innovations have led to the development of techniques which aim to improve the quality of the newly formed fibrocartilage covering which results from microfracture alone – this is described next.
- Mononuclear concentrate (MCC) in a platelet-rich plasma (PRP) matrix – this procedure involves using concentrated injections of the patient’s own platelets (present in blood plasma) to accelerate healing. This treatment begins with the harvesting of stem cells from the patient’s bone marrow, followed by taking some PRP from the patient’s blood. Microfracture is then performed, PRP is applied to the area of clot formation and, when this is stable, the previously harvested stem cells are inserted below the clot. This marks the end of the procedure, which is all completed as a single stage.
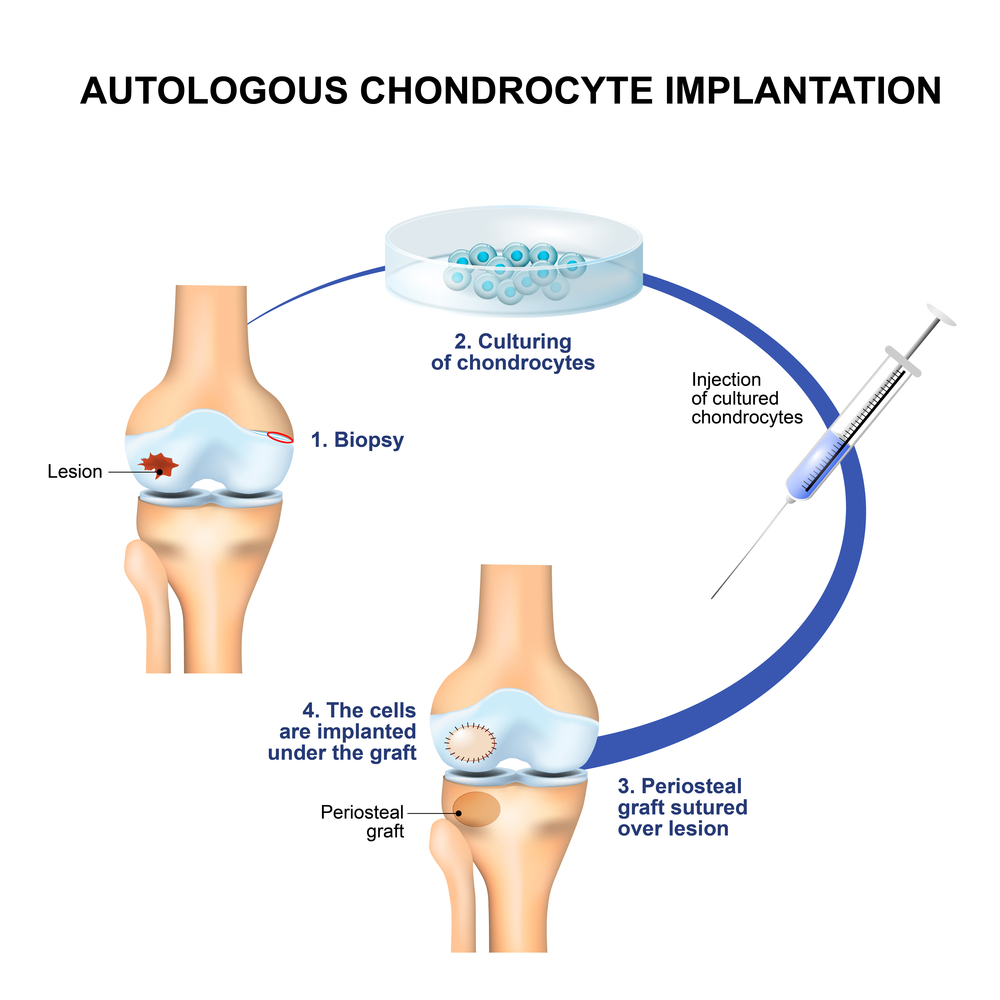
- MACI (matrix-induced chondrocyte implantation) – a range of methods exist, but most involve the removal of a small sample of cartilage cells (chondrocytes) from the affected area in the hip, which is then sent to a laboratory and used to grow a fresh supply of cartilage cells. These are then reimplanted to fill the damaged area. These procedures involve one or two stages, depending on the process used for the harvest of cartilage cells prior to reimplantation.
- AMIC (autologous matrix-induced chondrogenesis) – combines microfracture with the application of a collagen mesh/membrane which is used to cover the area where new cells have been released, protecting them during the period of new tissue growth. This is usually used to treat defects affecting the hip joint socket.
Osteochondral Defects
- Mosaicplasty and OAT (osteochondral autograft transplantation) – methods involving the use of osteochondral plugs (small, precisely cut plugs of tissue composed of articular cartilage overlying undamaged bone), which are harvested from the patient (autograft) and used for the treatment of smaller lesions of the femoral head.
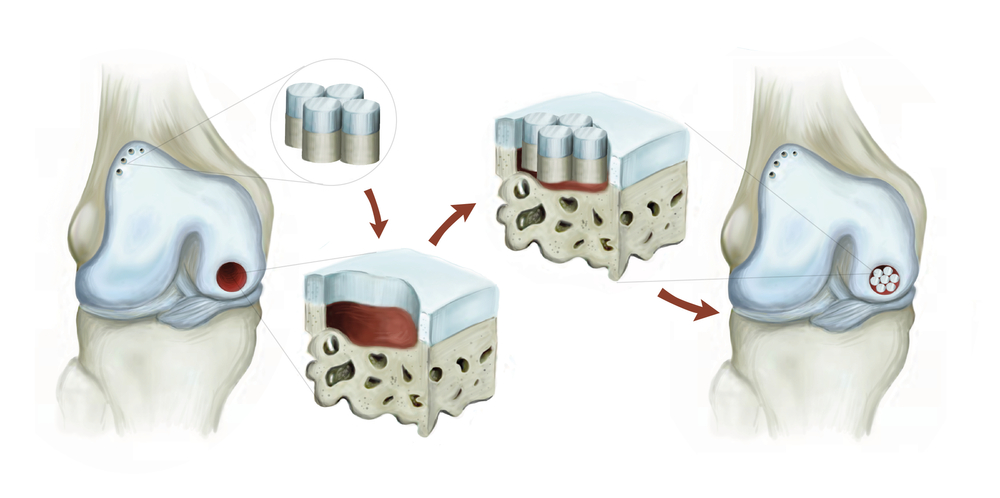
Note: The image above depicts a knee, but the principle of treatment is the same for the hip.
When harvested from the patient, the plugs are taken from a non-weightbearing area of the femoral head or the knee on the same side. These are single stage procedures, performed either arthroscopically, open or as a combined approach.
Mosaicplasty describes the treatment of multiple smaller sized lesions, whereas OAT is used for larger lesions – the process is otherwise the same for both. The risk of subsequent problems at the donor site is a disadvantage to this method. The area used may start to develop pain, more extensive degenerative changes, and ultimately osteoarthritis.
- OCA (osteochondral allograft) – this procedure is similar to the OAT and mosaicplasty methods, but the osteochondral plugs are taken from a donor (allograft). This removes the risk of donor site problems. OCA may be used to repair defects in both the femoral head or the acetabulum and may also be relevant in the treatment of patients who are young and have been diagnosed with avascular necrosis (AVN) or some degree of collapse of the femoral head.
What to expect after surgery
Recovery following cartilage repair techniques is usually slow as this tissue takes a long time to heal.
There will be limitations to weightbearing and activities during the first two or three months, which will vary amongst surgeons and will depend on operative findings and techniques performed. If microfracture is performed, partial weightbearing may be recommended for eight weeks to allow the bony surface to heal.
Physiotherapy can begin immediately after surgery, gradually increasing range of movement, stability, strength, mobility and function over a period of up to one year, depending on the surgery performed and individual aims.
References
Alison A Dallich, Ehud Rath, Ran Atzmon, Joshua R Radparvar, Andrea Fontana, Zachary Sharfman, Eyal Amar, Chondral lesions in the hip: a review of relevant anatomy, imaging and treatment modalities, Journal of Hip Preservation Surgery, Volume 6, Issue 1, January 2019, Pages 3–15, https://doi.org/10.1093/jhps/hnz002