Patient Information from ISHA – The Hip Preservation Society
Ligamentum Teres Tears and Other Soft Tissue Injuries
Ligamentum Teres Tears and Other Soft Tissue Injuries
There are many soft tissue injuries and conditions which may occur around the hip affecting bursaes, tendons, ligaments, and muscles. These are often treated non-surgically, but where surgery is necessary, consultation with a hip preservation surgeon is advisable, where thorough assessment and imaging are likely to be needed before a treatment plan is decided. Some examples of the structures which may be injured are described below.
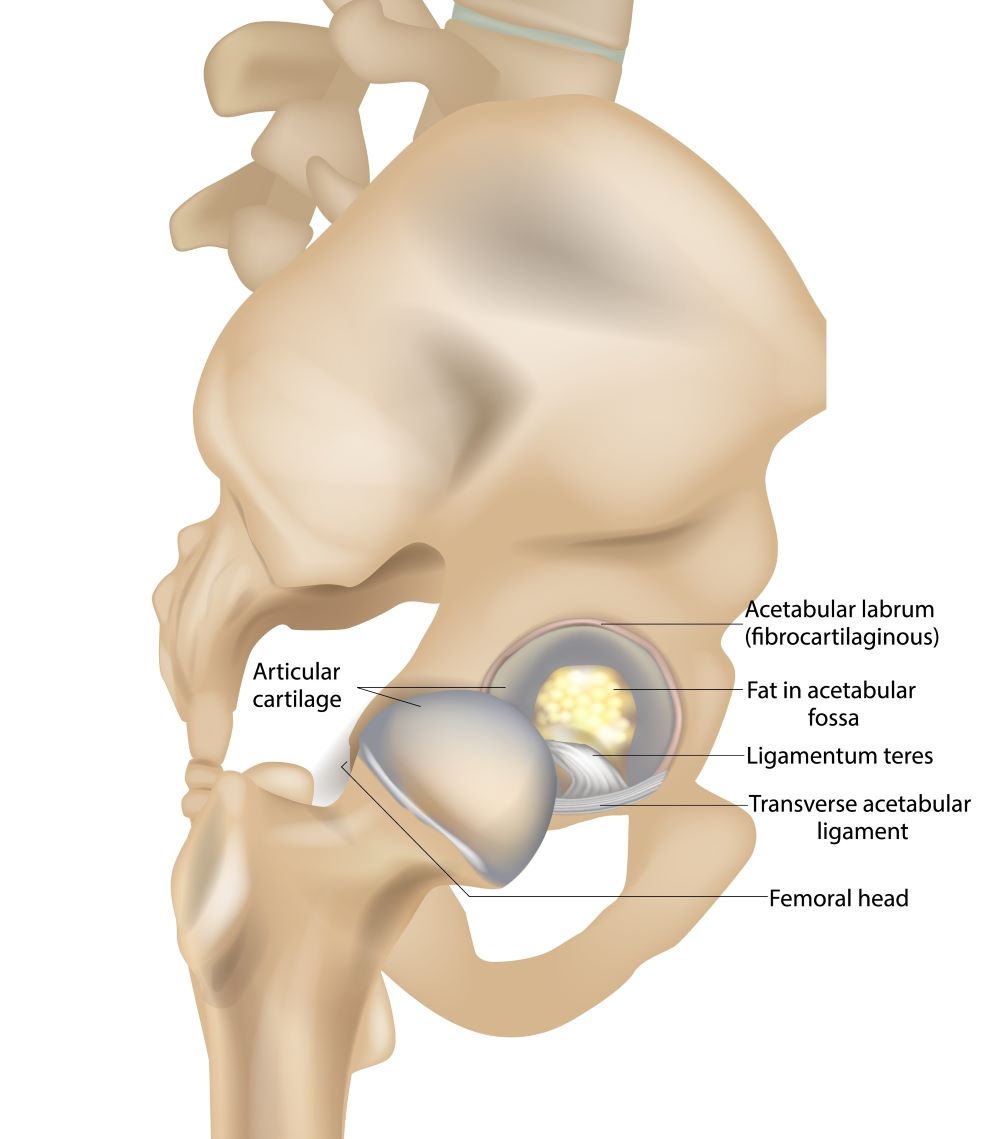
Ligamentum Teres
This ligament is a cord-like structure which attaches at one end to the head of the femur and at the other to the hip joint socket (acetabulum). This cord consists of two parallel fibrous bands and is thought to provide some stability to the hip joint by limiting excessive range of movement.
When torn, either partially or entirely, varying degrees of instability may result, causing pain and reduced mobility. There may be symptoms of clicking and locking. Damage to the ligamentum teres may result either from a traumatic injury such as dislocation, or from non-traumatic causes such as overuse, chronic irritation associated with other conditions such as femoroacetabular impingement (FAI), or hypermobility.
Tears are more often partial but complete ruptures are possible. Imaging may not reveal ligamentum teres injury and it may only be discovered during an exploratory hip arthroscopy when all other options for non-surgical treatment or diagnosis have failed. If found to be damaged, surgical treatment tends to involve removing and tidying any damaged tissue and/or reconstruction. The latter procedure involves replacing the damaged ligament with a grafted one, using part of the patient’s own hamstring tendon, for example.
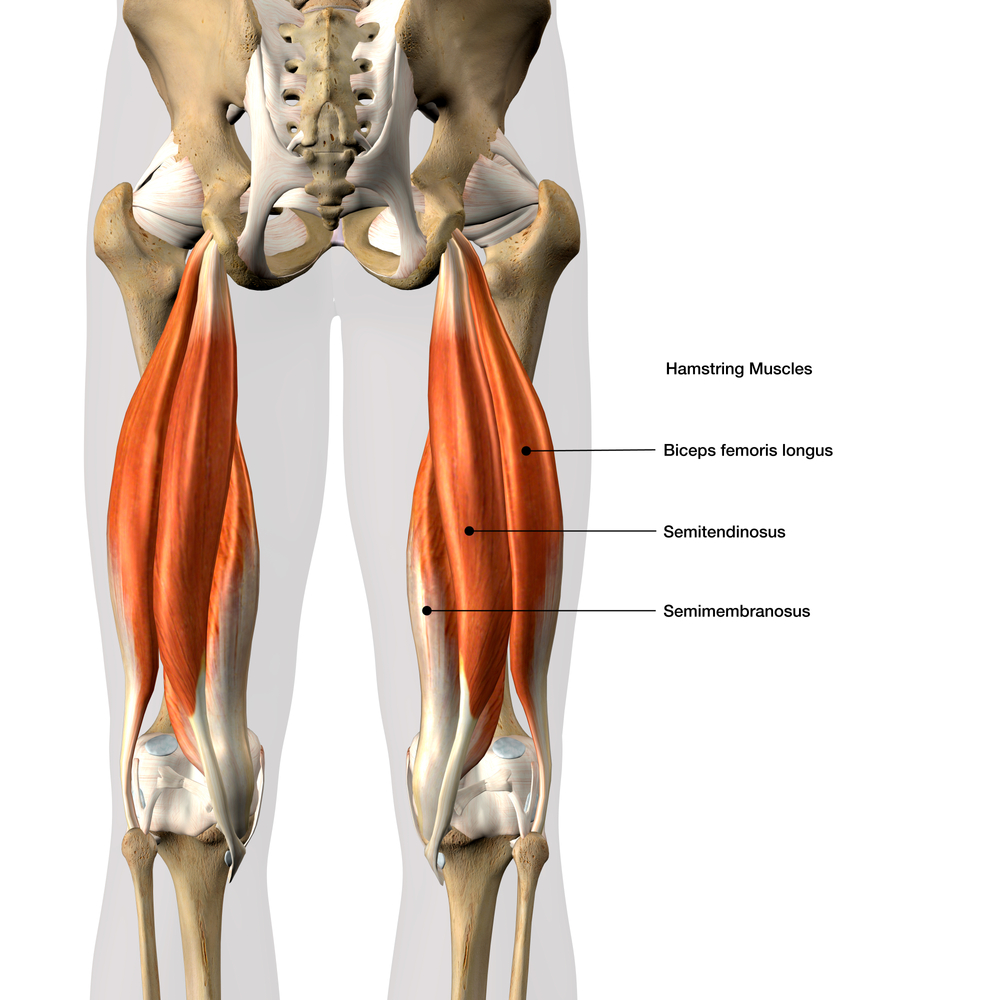
Definition
The three hamstring muscles are located at the back of the thigh. They extend from various attachments around the knee up to the ischial tuberosity (sitting bone). Injury to the hamstrings tends to occur more often in the sporting population, resulting in tears to varying degrees either where the muscle becomes tendinous (musculotendinous junction) or where the hamstring tendon attaches to the ischial tuberosity on the pelvis. Damage can range from minor strains to significant injuries, where the tendon detaches entirely from the ischial tuberosity; it may take a small piece of bone with it (avulsion fracture). Tendon damage can also occur from overuse injuries, where repetitive movements may cause the tendon to degenerate close to its attachment to the tuberosity.
Individuals who have torn one or more hamstring tendons may recall a popping or tearing sensation and present with significant bruising, pins and needles and loss of function. X-rays and MRI will often confirm the extent of soft tissue damage and whether any bony injury has occurred.
Non-Surgical Treatment
Physiotherapy can be effective for more minor strains and tendon conditions, and may involve use of ice, anti-inflammatory medication, rest and activity modification, soft tissue therapy and graded exercise programmes with a gradual return to pre-injury activities. More significant injuries may require surgical repair.

Surgical Treatment
During a hip arthroscopy, the ischial tuberosity can be reached, and any detached or torn tendons repaired and reattached. Any other soft tissue damage or areas of concern in the area, such as bursitis, can also be addressed. Some hip preservation surgeons may perform this procedure via an open approach instead of arthroscopically, for several reasons, including:
- the need for a graft;
- delays in performing reconstructive surgery;
- the development of scar tissue; and
- surgeon preference.
A period of rehabilitation will be required before returning to normal activities and sports. This is likely to involve a period of graded return to full weightbearing, with a gradual increase in range of movement giving any tendon repairs time to heal before regaining flexibility.
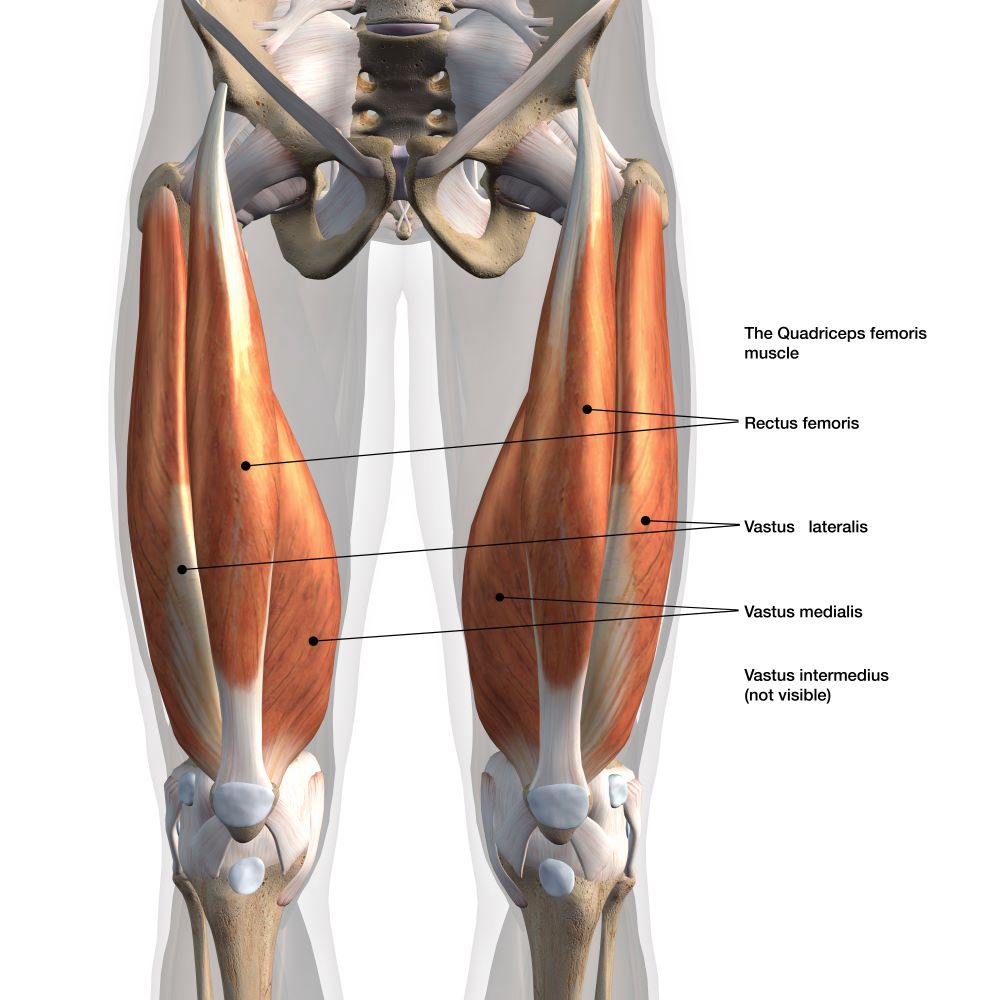
Rectus Femoris
The front of the thigh is made of four muscles, namely the quadriceps. These extend upwards from around the knee joint to attach at various points around the front of the pelvis and hip. The rectus femoris muscle is the largest of the four and is involved in straightening the knee and bending the hip joint. It can transmit large forces due to its size and so injury tends to occur during explosive actions such as jumping or sprinting.
Injury can occur in three areas of the rectus femoris:
- In the main muscle belly
- Where the muscle becomes tendinous
- Where the tendon attaches to the pelvis
Occasionally, and more often in younger individuals, the rectus femoris tendon may become completely detached from the pelvis, taking a piece of bone with it (avulsion fracture).
The severity of the injury will determine the best treatment required. Physiotherapy involving any combination of rest, ice, manual techniques, graduated exercise regimes and activity modification could be effective for most rectus femoris injuries. Where the tendon has torn completely or an avulsion fracture has occurred, surgical repair may be required. This would be followed by a period of rehabilitation, with the aim of returning to normal activities and sport.
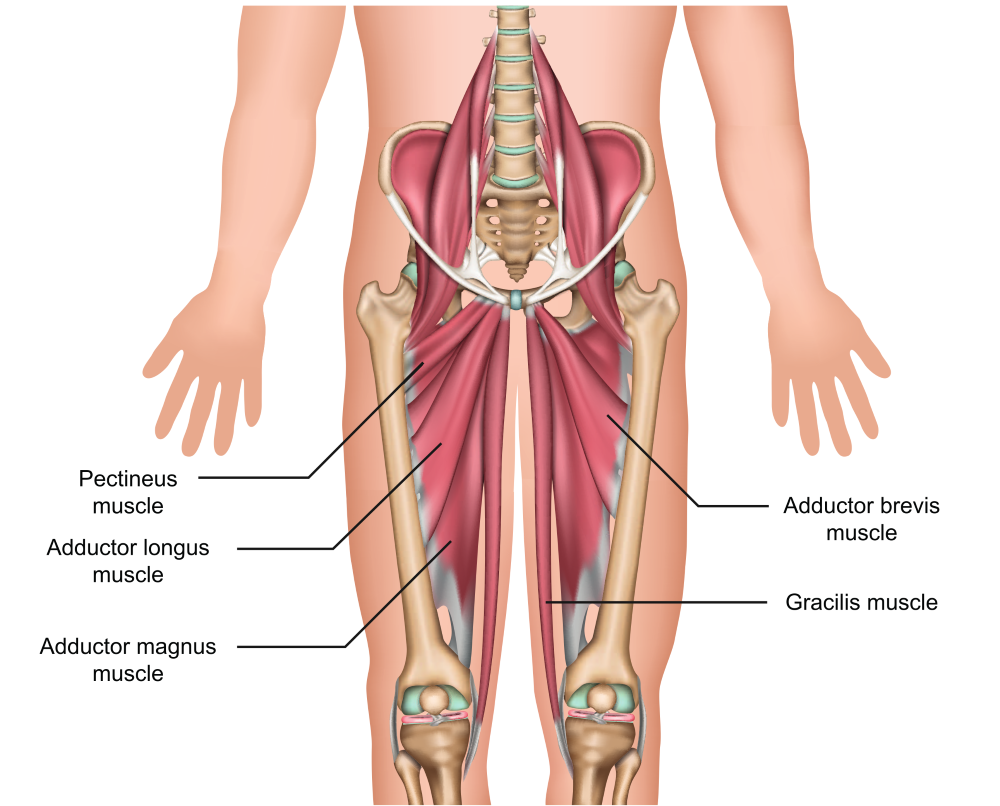
Adductors
The hip adductors are located on the inside of the thigh and are made of up five muscles, with the adductor longus the one injured most often.
Injury is usually the result of sporting activity. Non-surgical treatment is often effective, involving any combination of rest, ice, use of anti-inflammatory medication, manual therapy, exercise regimes and a graduated return to normal activities and sport. Surgical management may be required if chronic adductor tendon problems develop or if the injury is severe. Consultation with a hip preservation surgeon will take place, where a physical examination and imaging including X-ray and MRI will be reviewed prior to assessing whether any intervention is needed. This would be followed by a period of rehabilitation.