Patient Information from ISHA – The Hip Preservation Society
Hip Instability
Hip Instability

Definition
The hip is an inherently stable joint due to the following anatomical features:
- The shape of the bones (rounded femoral head, concave acetabulum and the angular shape of the femoral neck)
- The capsule, which is strong and reinforced by ligaments
- The labrum
- Most of all the 21 muscles which cross the joint at varying angles and locations
Damage to any of these structures may result in varying degrees of instability causing pain and an inability to perform normal activities. Hip instability can result either from trauma or hypermobility.
Traumatic Hip Instability
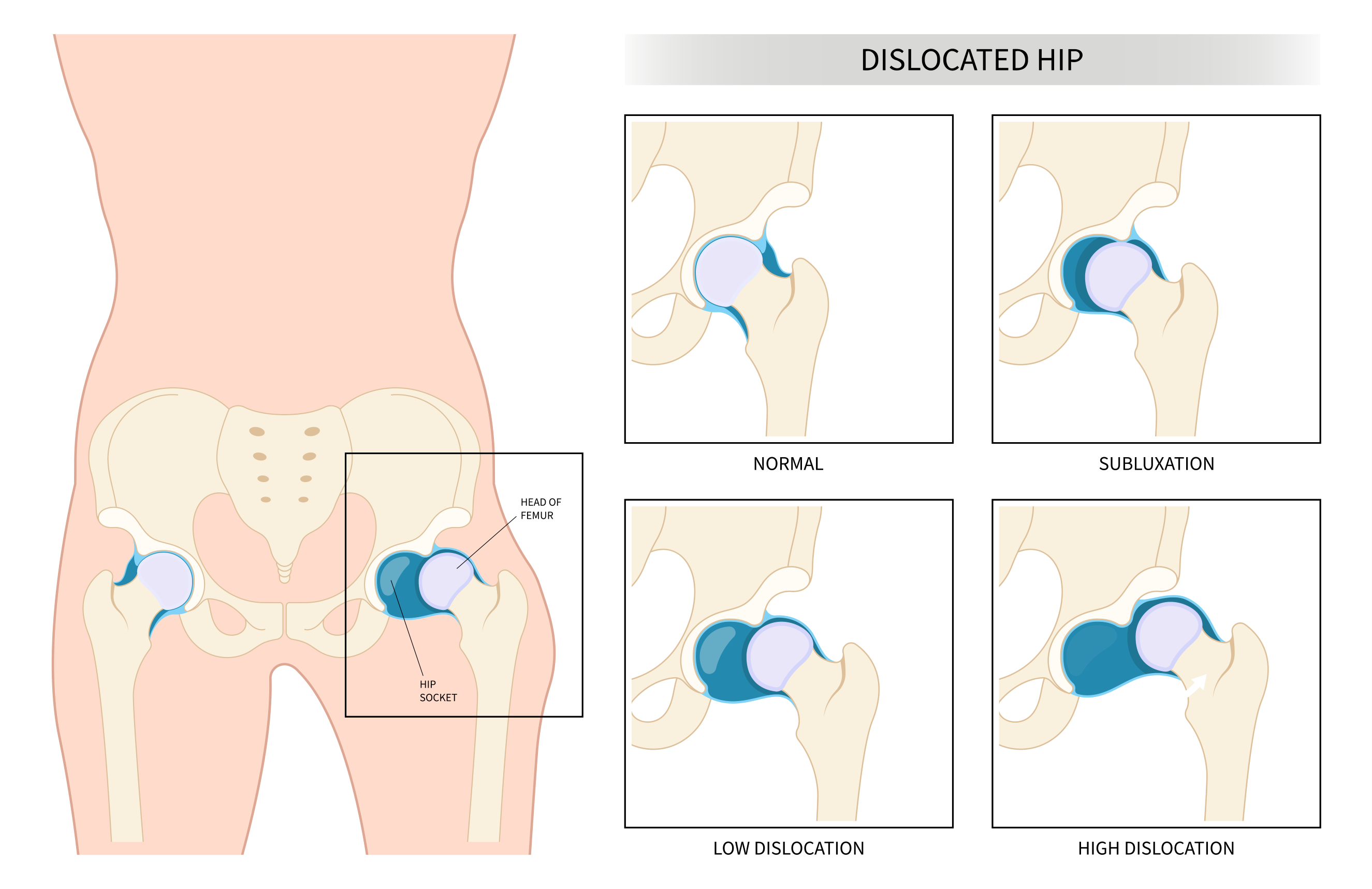
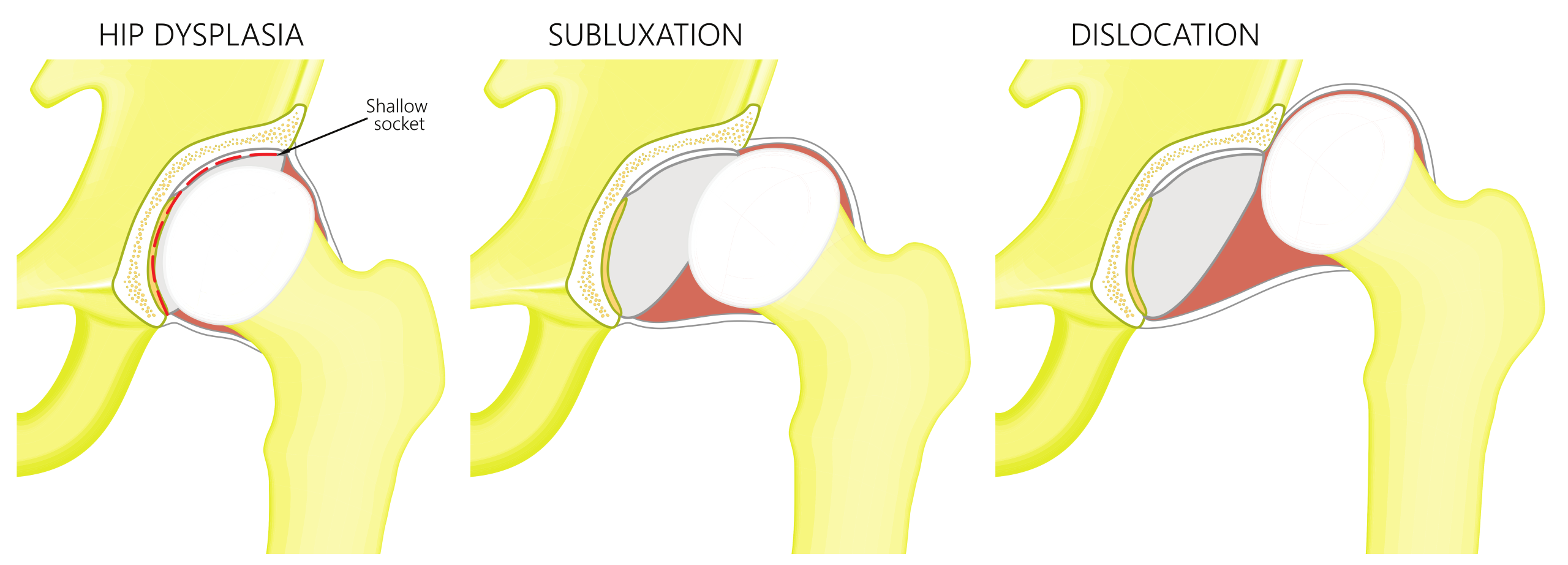
Traumatic instability may occur following a significant traumatic event, such as a road traffic accident, or from a sports injury. This can result in a full joint dislocation, which is rare, or varying degrees of subluxation (or partial dislocation), where the femoral head is not fully aligned with the acetabulum.
Dislocations, which are rare, may cause damage to the top of the femur, labrum, cartilage, and soft tissues (muscles, tendons and ligaments). Where this has occurred during a major traumatic event, treatment is likely to have taken place urgently and is not discussed further here. The long-term consequences of any such injury, however, may require later treatment and fall under the remit of hip preservation surgery. This could include surgery to the labrum, capsule, ligaments or tendons, or attention to any cartilage damage.
Atraumatic Instability
This occurs due to significant anatomical deformities seen in conditions such as hip dysplasia and other developmental hip diseases.
Microinstability
This describes conditions where there is too much movement of the femoral head within the socket. This increase in movement may cause damage to surrounding structures, resulting in labral tears and over stretched ligaments, causing yet further movement within the joint. The surrounding muscles work harder to keep the hip stable, resulting in inflammation, overuse and pain. Over time, the other hip compensates, resulting in weakness in the unstable side, further increasing the degree of instability.
Signs and Symptoms
- Pain, usually in the front of the hip or groin
- There may be mechanical symptoms, such as snapping, clicking, catching and popping
- Sensation of the hip giving way

Diagnosis
Diagnosis of microinstability can be difficult due to the wide ranging and sometimes non-specific signs and symptoms. The most frequent symptom is hip pain, which can also occur for many reasons including:
- Labral tears
- Cartilage defects
- Muscle weakness
- Ligament laxity
- Ligamentum teres damage
- Damage to the joint capsule, for example in previous hip arthroscopy surgery
- Subtle bony abnormalities
- Hypermobility of the hip, which could be the result of connective tissue disorders, such as Ehlers-Danlos syndrome
- Sports requiring repetitive actions, such as football, dancing or skiing
A detailed history will be taken, followed by a physical examination and imaging. Diagnosing hip instability can be complex and will require consideration of any past hip trauma or surgery, the presence of any hypermobile tendencies, an understanding of participation in sports, and the presence of any connective tissue disorders.

Non-Surgical Treatment
- Activity modification
- Use of non-steroidal anti-inflammatory medication
- Physiotherapy aiming to modify movement patterns by improving stability around the hip, pelvis and lumbar spine to help stabilise the joint and prevent the onset of pain during aggravating activities
Surgical Treatment
Treatment of any trauma-related instability where a full dislocation and other fractures or cartilage damage may have occurred will be treated by an orthopaedic trauma team at the time of injury. Surgery is likely to be open and may involve the use of metalwork including plates and screws. Where instability is deemed to be atraumatic or microinstability, surgical options can be wide-ranging, depending on which structures require attention. Any arthroscopic treatment could include any of the following, either in isolation or combination:
- Tightening of the joint capsule
- Reconstruction of ligaments (for example ligamentum teres)
- Repair or reconstruction of labral tears
- Microfracture to treat areas of cartilage damage
- Stem cell treatment for cartilage defects
- Correction of any bony abnormalities via osteoplasty, osteotomy
What to expect after surgery
Recovery following arthroscopic surgery is generally quicker than after an open procedure and hence returning to activities is also easier. Any return to sport will also depend on operative findings, and advice will be provided by the treating hip preservation surgeon and physiotherapist.
There may be limitations to weightbearing and activities during the first two or three months, which will vary amongst surgeons and will depend on operative findings and techniques performed. If microfracture is performed, partial weightbearing may be recommended for eight weeks to allow the bony surface to heal.
Physiotherapy can begin immediately after surgery, gradually increasing range of movement, stability, strength, mobility, and function over a period of up to six months, depending on the surgery performed and individual aims.