Patient Information from ISHA – The Hip Preservation Society
Avascular Necrosis (AVN)
Avascular Necrosis (AVN)
Definition
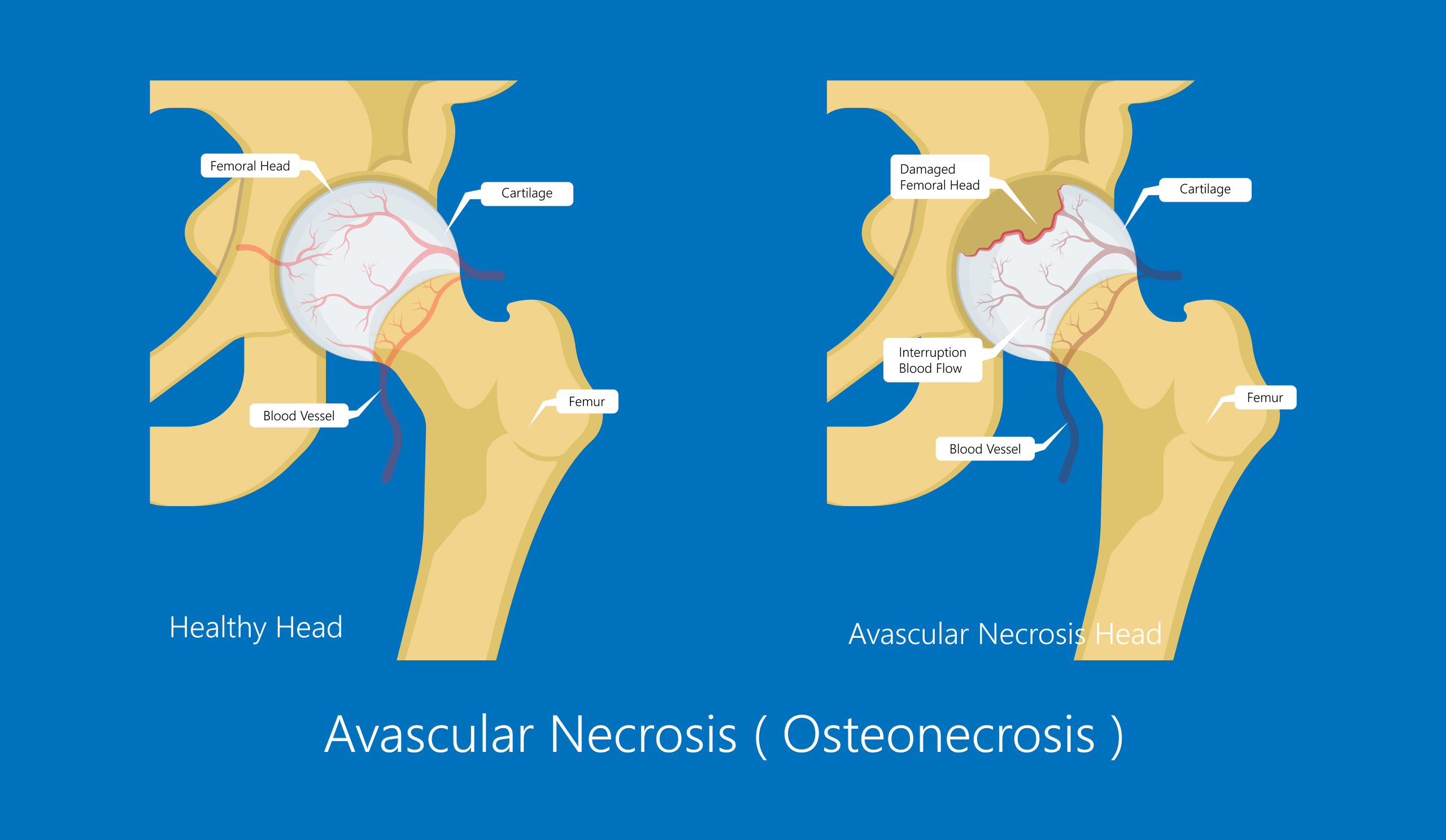
Temporary or permanent interruption of blood supply to the femoral head may result in varying degrees of damage to the hip joint. In the absence of a blood supply, bone cells cannot survive and consequently destruction of bone (osteonecrosis or avascular necrosis) may develop.
The femoral head begins to collapse and flatten, losing its normal rounded shape, and the hip joint is then unable to move normally, resulting in pain and stiffness. Where bone cells have been destroyed, the overlying cartilage may also begin to wear, and severe osteoarthritis may result. The only treatment would be a total hip replacement.
AVN is more common in males, and whilst it is most often seen affecting the femoral head, it may involve the knee, heel and humeral head (shoulder), as well as very rarely the wrist and jaw. Early diagnosis is essential to prevent complete collapse of the femoral head, which would require a total hip replacement. It may occur at any age and when seen in children is better known as “Legg-Calve-Perthes Disease” (or simply “Perthes Disease”). In children, however, the interruption to the blood supply does eventually recover spontaneously, with the process taking between two and five years.
The cause of AVN is generally unclear, but there are some known risk factors, including recent trauma, steroid use, autoimmune disease, sickle cell anaemia, alcohol abuse, smoking, and radiation treatment. More recently, COVID-19 was identified as a possible cause.
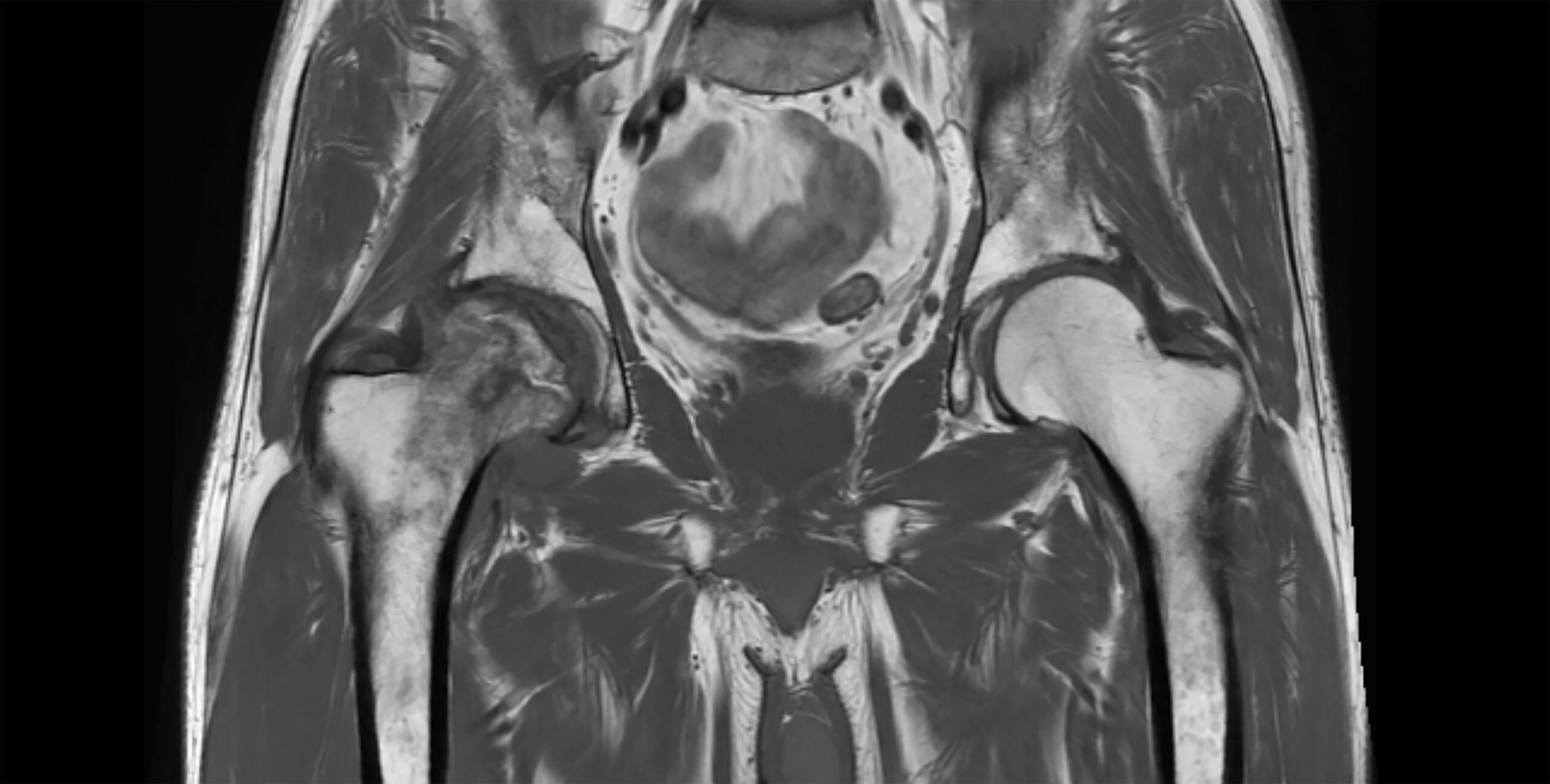
Image Right: Avascular necrosis confirmed by destruction of bone of the right femoral head
Signs and Symptoms
In adults, pain of varying severity may be the first sign something is wrong. Other symptoms may include:
- Limping
- Difficulty managing stairs
- Difficulty standing and walking
- Stiffness and reduced range of movement

Diagnosis
Following a detailed history taken by a hip preservation surgeon, imaging will be required. In the early stages of the disease, X-rays may not show any changes in the joint, so MRI tends to be used for early detection.
Non-Surgical Treatment
It can take some time before there is any relief from pain using non-surgical therapies and so most patients will opt for surgery. Research involving medicinal trials into the use of alendronic acid and bisphosphonates with the aim of preventing collapse of the femoral head and hence delaying progress of the disease remain inconclusive.
Surgical Treatment
There are some hip preservation procedures which may be helpful during the early stages of the disease, including:
Core decompression
Drilling into the area of damaged bone to stimulate blood flow, which may promote bone regeneration. This is sometimes combined with the use of bone marrow harvested from the patient, where stem cells can further stimulate bone healing. This procedure would be performed arthroscopically.
Femoral osteotomy
An open procedure, involving repositioning of the femoral head to remove weightbearing pressure from the area of bone destruction.
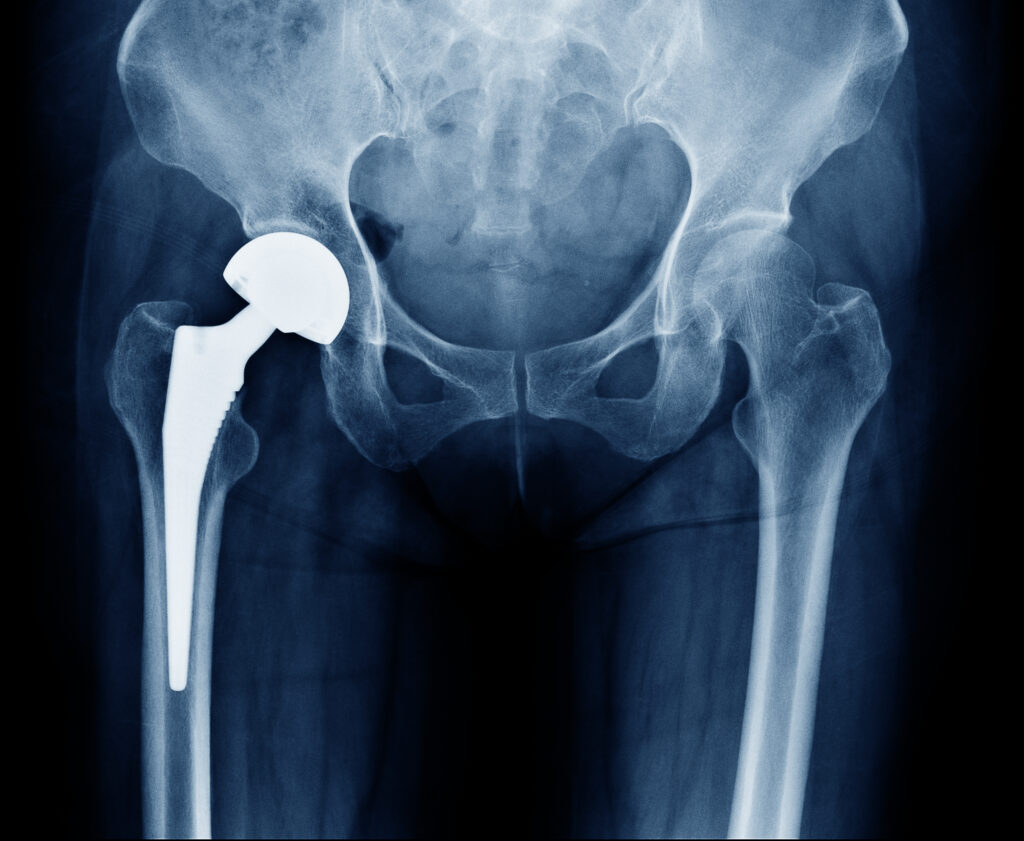
Total hip replacement
In the following circumstances, a total hip replacement will be the favoured treatment:
- Where the condition is deemed irreversible due to collapse of the femoral head
- Failure of previous hip preservation procedures
- In older patients with more extensive damage to the bone and cartilage which have resulted in the development of osteoarthritis
- In younger patients with significant damage to the femoral head and acetabulum
What to expect after surgery
This will vary depending on which surgery was performed and the preferences and recommendations of the treating hip preservation surgeon.
Following core decompression, weightbearing and activities are likely to be limited for the first six weeks. A programme of non-weightbearing exercises and hydrotherapy may be advised and supervised by a physiotherapist during this time. A graduated return to full mobility and activities will then be possible, with exercises to restore movement, strength and function.
Following a femoral osteotomy, there may be limitations to weightbearing and activities during the first two or three months. This will vary amongst surgeons and will depend on what is found during surgery and the techniques performed. Physiotherapy can begin immediately after surgery, gradually increasing range of movement, stability, strength, mobility and function, with the recovery time dependent on the surgery performed and individual aims.